By Josée Lavoie, CHU Sainte-Justine
Josée Lavoie is a dietician and has been Manager of Food Services at CHU Sainte-Justine in Montréal, Quebec since 2009. In 2016, CHU Ste-Justine made a major shift through a room service program to allow patients to choose what they want to eat and when they are hungry. Josée’s goal as a Nourish innovator is to increase the quantity of local Quebec foods on menus and to become more eco-friendly.
Food Services Modernization Project
CHU Saint-Justine, one of Quebec’s two children’s hospitals, undertook a major food services modernization in 2011, when the hospital decided to revise its practices in order to counteract high meal dissatisfaction rates (60%) and high uneaten meal rates (25%), which resulted in food waste to the tune of $89 000. The project aimed at re-engineering the hospital’s food services, with a view to:
- making services more human-oriented;
- improving satisfaction rates;
- facilitating the nutritional management of clients; and
- ensuring optimal efficiency (human, ergonomic and financial).
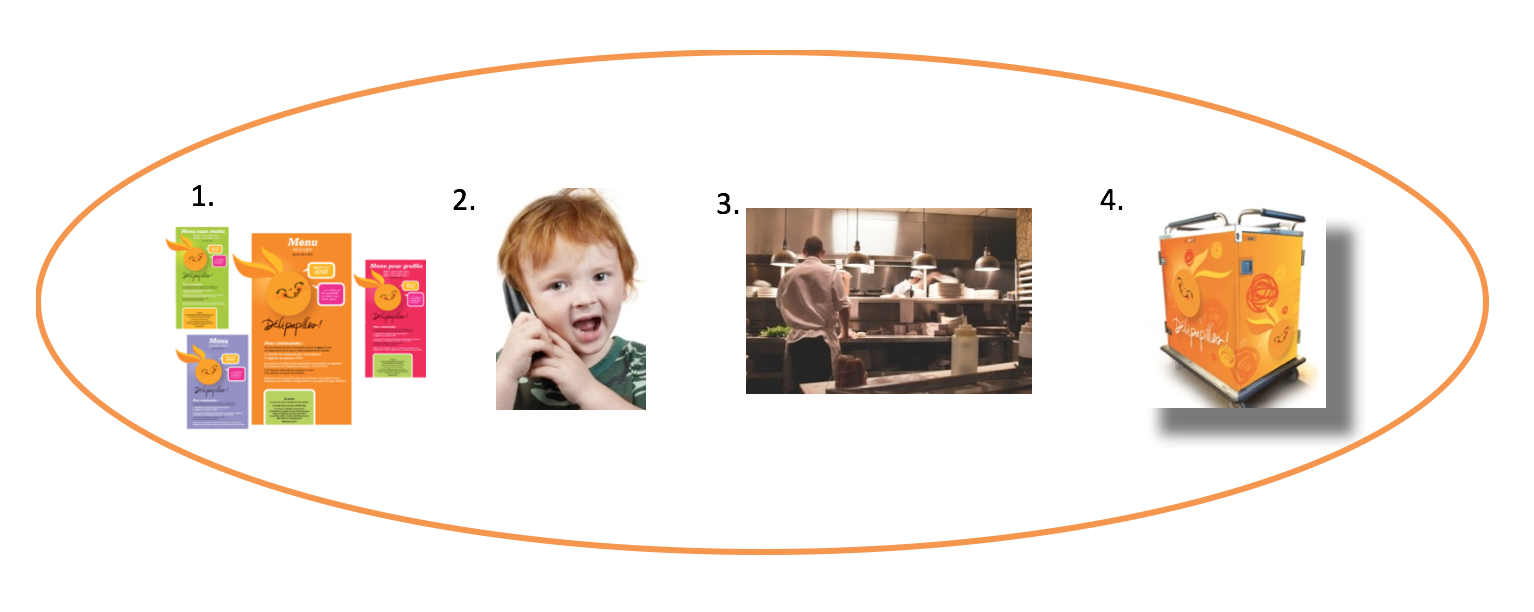
Visual identity of Délipapilles Room Service
Food service evolved from a traditional heat-preserved meal service with a strict service schedule to a just-in-time system, in which food is prepared and trays are delivered at the convenience of patients, who can regain control of their diet by choosing what they want to eat and when they want to eat it. This shift in culture was made possible by the approval from all of the organization’s steering committees and, most importantly, the cooperation from all units. Several facets of the project were then developed simultaneously; these included drafting architectural plans and renovating the kitchen, revising processes, designing menus, establishing operating procedures, developing software and creating a visual identity in the CHU St Justine’s colours.
Who Can Order Meals?
All patients, including those with complicated dietary restrictions, can order meals. Five menus were created in an effort to meet all types of dietary restrictions: regular, transplant, low residue, kosher and glycogen. Each order is processed by a dietary technician. Meal delivery service is currently being extended to parents and all hospital employees.
How Does It Work?
Patients choose from an à-la-carte menu (1) and phone a technician to place their order (2). About 45 minutes later, a freshly prepared meal (3) is delivered to their room (4). Patients, their parents or the care team may order the meals ahead of time, from the hospital or from home. Everything has been designed to offer a flexible service that is adapted to the needs of clients, whether it’s a plate of pasta for a mother who has just given birth or a bowl of cereal for a toddler to snack on just before bedtime!
Organizational Culture: Putting the Patient at the Heart of Our Concerns!
A direct result of the 2011–2014 strategic plan drawn up by the CHUSJ’s management team, room service has proven to be a massive project requiring an analysis of key project management processes. The project is connected to the "quality and safety" and "modernization" elements of the strategic plan, both for the food served to clients and the work environment. It also reflects the organization’s culture (discovery, innovation, accountability). Room service is essentially a patient-centred means of distribution, which places the patient at the heart of the process.
And So It Begins!
The project was launched on January 19, 2016. Since then, all hospitalized patients (except psychiatric clients and those with eating disorders) can choose what they want to eat for meals and snacks any time between 6:30 am and 7:00 pm.
Our performance indicators speak for themselves:
Are we proud of these results? Absolutely!
The Délipapilles Room Service Team
The entire food services team (cooks, food services staff, dietary technicians, technical assistant chefs, etc.) joined forces to successfully bring this innovative, personalized service to the hospital’s patients. It is worth emphasizing that we could not have done it without the participation of the care teams in presenting the service to clients. We are grateful to have them as our spokespersons.
Several other Nourish innovators have also been leaders in their facilities putting room service models into action with similar results of improving patient satisfaction and decreasing food waste and cost including:
Bernice Wolfe, Director of Food and Marketed Services, at the Children’s Hospital of Eastern Ontario which piloted room service model back in 2003. “Getting children to eat well is hard at the best of times. Children who are undergoing certain treatments often have irregular eating habits and decreased appetite. By responding quickly to their needs, we can better ensure that they are eating well which contributes to their recovery.” Families can order any menu items for their children from 8 am to 7 pm and meals are delivered in 20 minutes. Patient satisfaction is currently at 98%.
Nourish innovators Tina Strickland and Brenda Macdonald are working toward implementing room service at Nova Scotia’s largest hospital, the Halifax Infirmary. Dial for Dining, a 24-hour room service model, was launched in 2008 at the IWK Health Centre in Halifax, NS and at many regional Nova Scotia Health Authority sites across the province shortly thereafter. The implementation of Dial for Dining at the IWK resulted in increased patient satisfaction (90% patient satisfaction), and a 92% decrease in plate waste. (Watch a video about the initiative). Similar results were also achieved at other provincial sites that implemented a room service model. Visitors and staff can also order meals and enjoy this option.
Marianne Katusin, Manager of Food Services at Oakville Trafalger Memorial Hospital, in Ontario, initiated the “Call to Order” room service food delivery model for its Maternal Child and Medical/Surgical units in 2011. In addition to patient satisfaction increases (from 78% satisfied pre-room service to 96% satisfied with room service) they also experienced cost savings from eliminating the need for replacement trays and reducing unnecessary waste for an estimated 7% of raw food costs, which are approximately $900,000 annually.
Room service models are an exciting innovation towards more patient-centred food services and open the door for a deeper dialogue about how we can provide better hospital food for patients that also generate broader social, economic, health and environmental impacts.