Our Food Services Modernization Project saw the light of day in 2011, when the hospital decided to revise its practices in order to counteract high meal dissatisfaction rates (60%) and high uneaten meal rates (25%), which resulted in food waste to the tune of $89 000. Read more.
Letting Patients Guide Our Actions: Food for Thought!
Not everyone equates hospitals as a place for a pleasant dining experience, but the Nutrition and Food Service (NFS) team within Alberta Health Services is aiming to change that perception! Operating food services at 107 sites, NFS aims to put patients and their families at the centre of everything they do. Read more.
The Long and Winding Road – Creating a New Story of Hospital Food
By Stephanie Cook, Regina Qu’Appelle Health Region, Saskatchewan
Stephanie Cook is the Director of Nutrition and Food Services for the Regina Qu’Appelle Health Region. She is passionate about food and nutrition and has spent the last two decades leading initiative aimed at improving nutritional well-being, such as programs for overweight children, developing healthy food policies and combating malnutrition in hospitalized patients.
Ringo Starr does not seem pleased with his hospital meal.
It’s hard to pinpoint that place in time when hospital food, once a cornerstone of treatment and recovery and considered wholesome and healing, changed in the public’s opinion to its current lackluster reputation. I suspect it has steadily declined as medical science and technological advancements began to trump food as the primary therapy and budget expense. I can’t say for sure what Ringo Starr was thinking when this photo was snapped in 1964, but if his expression is any indicator, I think he was less than impressed with what was on his plate. Fast forward more than half a century later and the perceived dissatisfaction with hospital food is only growing, with those consuming it not shy about sharing their discontent. Any patient with access to a cellphone can take a photo of their meal and post it online, sometimes creating nothing short of a media firestorm about the deplorable state of hospital food.
“But then, I wondered, is the food really that bad or is its reputation so tarnished by rhetoric that we never considered the possibility it could be anything different?”
For years I believed it too - hospital food sucks. In my time as a clinical dietitian I would nod, knowingly and sympathetically, as staff joked and patients complained about the food. What could I do? This is a hospital, a publically funded institution with an ever-shrinking food budget and fewer staff to prepare it. With pre-packaged out-sourced foods and fancy re-therm equipment taking the place of real cooking from scratch, of course food quality suffered. How could we be expected to strive for anything more than mediocrity? But then, I wondered, is the food really that bad or is its reputation so tarnished by rhetoric that we never considered the possibility it could be anything different? Was it possible that any attempts at quality improvement were simply going unnoticed, mired down by an impenetrable narrative? When I looked around I saw many patients cleaning their plates and asking for larger portions. Considering that the context is a hospital, where people are sick, away from home and family, in a strange and sometimes frightening environment; I had to wonder, is the food really that bad?
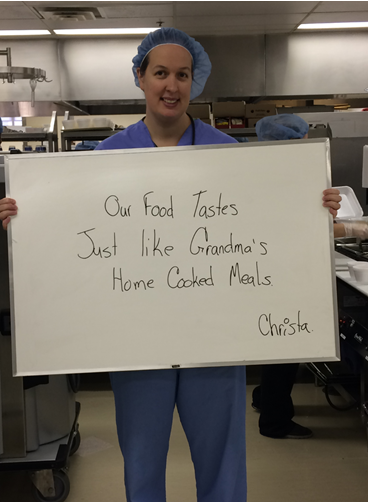
Admittedly, the food served in hospitals may not be exactly like our grandmothers. However, think about the task at hand - serving patients, most of them unwell, with different food preferences, coming from different cultures, and with varying nutritional needs — that’s no small feat! So when we put this in perspective, is the negative narrative that engulfs hospital food warranted? Or, is it simply a self-fulfilling prophecy? If we think that what we are about to eat is going to be terrible, then chances are it will be.
This issue bubbled to the surface in my health region not long ago when the results of the Canadian Malnutrition Task Force clearly identified how prevalent malnutrition is in hospitals and the many barriers that prevent patients from getting the nutrition they need. This led us to re-look at our food and assess is it really that bad or are we, hospital employees, so committed to the notion that hospital food is terrible that we unwittingly create yet another barrier that prevents patients from eating well?
4 dietitian students who were running the empty carts back to the kitchen to restock their supply of food (they had planned for about half as many participants!)
We devised a plan to try to measure this. The first step was surveying hospital staff to see what they thought. Predictably, staff rated the food negatively, describing it as unappetizing, lacking nutrition and of poor quality. As our second step, we decided to conduct a blind taste test in order to solicit more unbiased reviews. We advertised throughout the hospital that we were trialing some new items for our cafeterias and invited staff to sample six different entrees and rate their level of satisfaction (and ended up testing a total of 352 portions – reminding us to never underestimate the power of serving free food!). What we didn’t tell participants was that these were six entrees regularly served to our patients. The results were surprising with over 85% of participants indicating the entrées were “good”, “very good” or “excellent” for all quality measures (smell, taste, appearance, healthiness and overall acceptability). What’s more, over two-thirds of staff indicated they would purchase these entrees if they were offered in the cafeteria. That’s right, actually pay money for the very same meals we serve to our patients!
We have had a lot of fun sharing these results both within and outside of our health region. However, the greatest value without question has been sharing our findings with the food services staff. The positive reviews have helped validate what they know to be true — that every day they prepare and serve good food and they are proud of what they put on the plates.
This is not to say we don’t have opportunities to improve. In fact, listening to our patients was key to having our food so well-received. Patients have suggested they want to see more wholesome comfort foods made from fresh ingredients on the menu. While this sounds like a tall order, especially for hospitals that rely heavily on pre-prepared foods, there are a number of relatively simple fixes that can make a big difference. For example, in my health region we recently changed from buying pre-made broth soups to making them from scratch. We chose to focus on soup because it is a comfort food, fits most therapeutic diets and tends to be universally well-liked. We also saw an opportunity to pack in more nutrition using big pieces of vegetables, fresh herbs, noodles or rice and more protein. Not only do our patients approve but food services staff members feel good about making and serving it. We are also finding opportunities to include more locally grown foods on the menu, and spread the word to our patients and staff about our commitment to building a more sustainable food supply. Inviting staff to “come dine with us” and enjoy the patient meal of the day is another way to start engaging others.
“Bridging this gap is going to take more than just improving food - the healthcare sector needs a new commitment and an updated story of what goes on the plate, and how meaningful this can be to patients.”
In order to combat the long-time negative stereotypes surrounding hospital food, we must recognize the gap between where we are and where we want to be. Bridging this gap is going to take more than just improving food - the healthcare sector needs a new commitment and an updated story of what goes on the plate, and how meaningful this can be to patients.
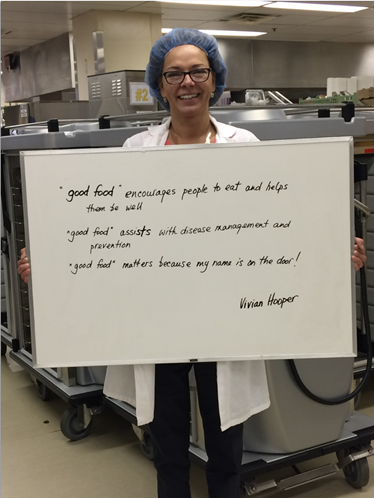
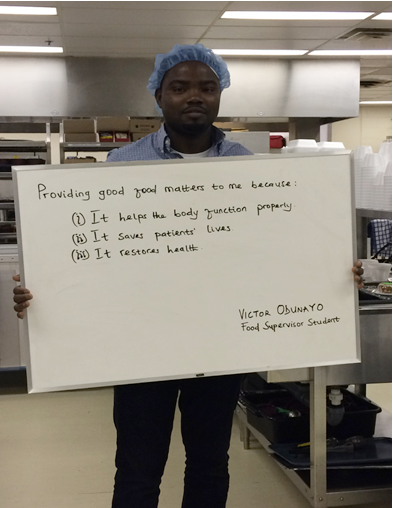
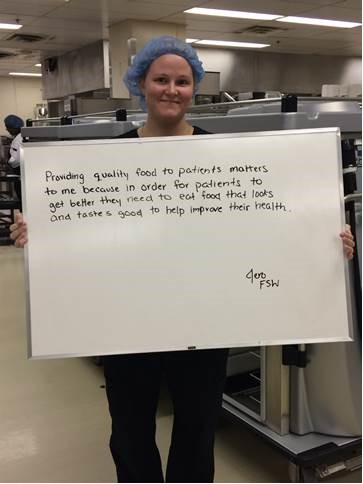
I asked staff at one of our hospitals the question “why does serving good food matter to you?”. No matter how they said it, the message was clear. Food is medicine and medicine heals.
Join me in creating this new story of hospital food!
Converging Around Collaborative Projects
On Friday, October 20th, the Nourish cohort is hosting a webinar to share and discuss its five collaborative projects around the future of food in health care. Register here.
One wicked, persistent problem in Canadian health care connects the twenty-five Nourish Innovators: the disconnect between food and health. The problem is a wicked one for the many ways it manifests, evolves, and refuses to go away, despite the common sense that nourishment is needed to be well and to heal.
The Nourish cohort spent the first months of the program unraveling the problem, reflecting on how it manifests at their respective organizations, in their supply chains, and across the Indigenous, French, and English populations they serve. They detailed their visions for the future of food in their organizations, and set out goals on the path to get there. Then over the summer, the cohort converged around a suite of collaborative, national projects to undertake across their organizations. This suite of complementary projects address some of the key barriers and points of leverage in the food and health systems.
The Process
The process was a dynamic, iterative one; an experiment in remote, virtual collaboration. $100,000 of funding was on the table for the cohort to decide how to use.The twenty-five Innovators internally generated fourteen project ideas, selected seven to develop, and pitched five. The cohort, advisors, and mentors provided feedback and recommendations that led to a refinement of the project ideas. A decision about how to allocate funding to the suite of projects was just confirmed, and the cohort will be sharing the announcement on an October 20th webinar to invite engagement with their work.
To borrow the reaction of one of our cohort members, "I am impressed with the group working together, with different objectives, to arrive at some unified goals." It was impressive. I watched the teams negotiate their own project scopes to guarantee funding for other teams. I got shivers. Special thanks go to our friends at MaRS and at Health Care Without Harm for acting as provocateurs in the early audience, and to all the mentors and advisors who are supporting the teams and helping to frame the big picture.
The Projects
Each of the five project teams will be approaching a different dimension of the disconnect between food in health care. The composition of the teams represents multiple provinces and territories, and the teams aspire to put in motion work that will be felt nationally. They are undertaking work to better understand the patient experience of food in health, and to address barriers to sustainable, local, and traditional food that supports health and healing. Specifically, their work relates to:
- Increasing the sector's ability to deliver Traditional & Country Food Programs for Indigenous patients and residents
- Developing a Sustainable Menu Guide to help the sector decrease its ecological impact and support social and economic wellbeing
- Creating a more enabling policy environment for a Food is Health approach in health care
- Developing National RFP Models for values-based healthcare food purchasing
- Researching strategies for benchmarking National Patient Satisfaction/Experience with Food Services
These collaborative projects fit into the broader work of Nourish to transform how we value and engage with food in care. They are ambitious, and provide an entry point for any fence-sitters who have been wondering - or waiting for! - a moment to jump in with Nourish.
We invite you to join us online on on Friday, October 20th at 1pm ET for the public kickoff of the projects. In addition to sharing their work, each team will share their invitation for feedback, and offer ways to engage with and support their projects.
We hope you will join us!